Cardiac risks associated with C-reactive protein levels are as follows [1] :
Low: < 1.0 mg/dL Average: 1.0-3.0 mg/dL High: >3.0 mg/dLHs-CRP appears within 1-2 days of acute myocardial infarction, peaks at 3 days, and becomes negative after 7 days. [2] Failure of CRP to return to normal signifies tissue damage in the cardiac or other tissues. The absence of a CRP increase in 2-10 days following the event raises the question of prior necrosis. [2] CRP does not usually increase in patients with unstable angina. Hs-CRP correlates with peak creatine kinase-MB (CK-MB) following acute myocardial infarction. CRP may remain high for at least three months following acute myocardial infarction. [2]
Increased in [2]
Acute or chronic inflammatory conditions
Tissue necrosis or tissue injury
Ischemia or infarction of issues
Malignant tumors especially of breast, lung and gastrointestinal tract
Hormone replacement therapy
In a report on older Black adults (aged 51 years or older), Farmer et al found elevated CRP in more than half of the study group’s women, with the increase indicated to have links to such factors as younger age, Medicaid, religiosity, overweight/obesity, physical inactivity, and activities of daily living (ADLs). A lower incidence of elevated CRP (37.25%) was found among Black men, with religiosity, reduced neighborhood cohesion, current smoking, overweight/obesity, ADLs, and more chronic conditions being associated with these higher levels. Moreover, among men, financial distress was linked to a decreased risk for high CRP. [3]
Exercise, weight loss, moderate alcohol consumption, medications like statins, niacin and fibrates [2]
Sex and race affect the CRP levels. African Americans have higher level than Caucasians and women have higher values than men. [2]
See the list below:
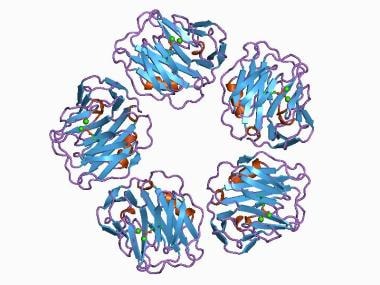
Specimen: Whole blood-serum, plasma Collection: Red top/ serum separator tubeCRP -- an acute phase serum protein – is a surrogate for the pro-inflammatory interleukin IL-6. [4] It is a member of pentraxin family of proteins and is synthesized by liver. [5, 6] CRP is also produced by cells in the vascular wall such as endothelial cells, smooth muscle cells, and also by adipose tissue. [2, 4]
It was discovered by Tillett and Francis in 1930. [7] CRP is a 224-residue protein with a molecular weight of 25106 Da. The CRP gene is located on chromosome 1. [8] CRP was so named because of its capacity to precipitate the somatic C-polysaccharide of Streptococcus pneumonia. [5] It has no relationship with protein C or C-peptide. It activates the complement system and binds to Fc receptors. [4] Significant rise in CRP indicates clinically relevant inflammation, and in contrast, the absence of a high CRP helps in exclusion of infection/inflammation. [4]
Sequential CRP may provide a more accurate assessment of inflammatory changes in response to treatment. CRP is very helpful in assigning a non-inflammatory cause to a markedly abnormal ESR. As for instance, in a patient with a monoclonal protein without any evidence of infection, ESR may be high (in 100) but CRP will be normal. [4] One should be cautious about the interpretation of CRP levels. CRP changes with body mass index. The new ultrasensitive CRP assays expressed in markedly different concentrations may be very confusing to the unwary. [4]
An image depicting C-reactive protein can be seen below.
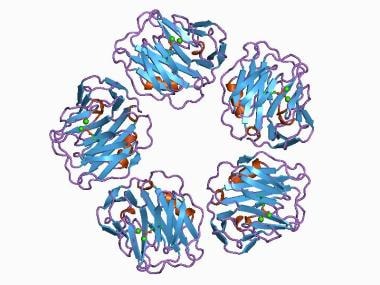
--> C-reactive protein, pentraxin-related.
Chronic inflammation is pivotal in heart disease; studies have shown that high levels of CRP, measured by hs-CRP, can be a marker of atherosclerosis. hs-CRP is an important predictor for cardiovascular events, including myocardial infarction, cerebrovascular events, peripheral vascular disease, and sudden cardiac death in individuals without a history of heart disease. In patients with acute coronary disease, CRP level predicts mortality and cardiac complications. [5] High CRP levels augur a worse prognosis in patients with acute coronary syndromes. hs-CRP is also a marker of metabolic syndrome. [6]
See the list below:
CRP - Suspected inflammatory state (vasculitis, autoimmune disorders, SLE, psoriasis, infection) CRP may sometimes be ordered along with erythrocyte sedimentation rate (ESR)CRP may be ordered, for example, when a newborn shows signs of infection or when an individual has symptoms of sepsis, such as fever, chills, and rapid breathing and heart rate
CRP may also be ordered to monitor conditions such as rheumatoid arthritis and lupus and is often repeated at intervals to determine effectiveness of treatment
hs-CRP can be ordered for patients with some established risk factors of coronary heart disease to determine strategy for prevention of cardiovascular events and for follow-up of patients with acute coronary syndromes
CRP, being a marker of acute inflammation, is elevated 100-1000 fold after infection or trauma and, thus, for its utility as a cardiovascular risk marker, needs to be measured 2 times at least 2 weeks apart, in a metabolically stable state, post infection or illness, since its half-life is 19 hours. Universal hs-CRP screening is currently not warranted except in patients with an intermediate-high Framingham risk score.
The median baseline level of CRP for young adults is 0.8 mg/L (the 90th percentile is 3.0 mg/L, and the 99th percentile is 10 mg/L). [9] However, CRP levels may increase from less than 50 μg/L to more than 500 mg/L, that is, 10,000-fold, following an acute-phase reaction. [5] The baseline CRP increases with age and with body mass index. Some laboratories provide a choice for a routine CRP assay (suitable for the detection and monitoring of inflammatory disease) versus a highly sensitive CRP assay for the determination of cardiac risk. [10] CRP level is useful both in the clinical assessment of chronic inflammatory disorders and assessment of vascular inflammation, and therefore, in cardiovascular risk stratification. CRP level has been found to be an independent risk factor for atherosclerotic disease. In patients with coronary artery disease, high CRP level is associated with increased cardiovascular morbidity and mortality. High sensitivity CRP (hsCRP), a marker of systemic inflammation, has been identified as a valid biomarker of cardiovascular risk. [11] The best evidence to date supports the use of hs-CRP as an independent predictor of high risk for coronary artery disease. [12] The cut points of low risk (< 1.0 mg/L), average risk (1.0 to 3.0 mg/L), and high risk (>3.0 mg/L) correspond to approximate tertiles of hs-CRP in the adult population. The low-risk tertile has about half in relative risk compared with the high-risk tertile. [12]
CRP rises rapidly reaching a peak in 2 days during an acute phase reaction. CRP decreases rapidly with the resolution of the acute phase response (with a half-life of 18 hours). High CRP level does not have diagnostic specificity, as a large number of clinical conditions increase CRP. A high CRP lends support for suspected inflammatory disease, such as giant cell arteritis or polymyalgia rheumatica, when other features are sparse or absent. CRP more than 10 mg/L indicates clinically significant inflammation. Therefore, monitoring CRP levels may provide useful information on the diseases activity such as flare up of rheumatoid arthritis and giant cell arteritis. [10] However, elevations of CRP may occur in renal failure even without clinically significant inflammation. CRP usually does not increase (may be a slight rise) in scleroderma, polymyositis, and dermatomyositis. CRP levels also tend not to be elevated in SLE unless serositis or synovitis is present. [10]